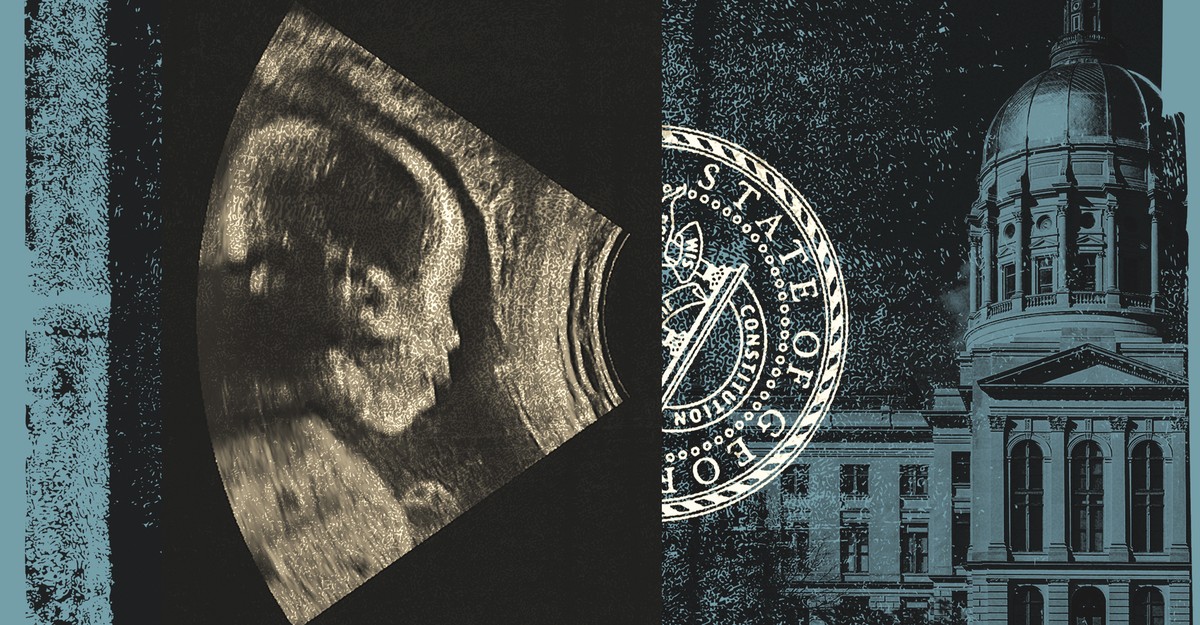
In the early hours of June 13, a baby was born to a brain-dead woman in Atlanta. That woman, Adriana Smith, had suffered a catastrophic stroke in February, in the early weeks of her pregnancy. When the baby, Chance, was born via C-section, he weighed less than two pounds. Last week, doctors at Emory University Hospital, where Smith was initially declared brain-dead, turned off the machines that had been sustaining her organs—and finally returned her body to the care of her family.
在6月13日凌晨,一个婴儿出生于亚特兰大的一名脑死亡女人。那个女人阿德里亚娜·史密斯(Adriana Smith)在怀孕的早期几周就遭受了灾难性的中风。当婴儿(Chance)通过剖腹产出生时,他的体重不到两磅。上周,史密斯(Smith)最初被宣布为脑死亡的埃默里大学医院(Emory University Hospital)的医生关闭了维持她的器官的机器,并终于将她的遗体归还给家人的照顾。
Usually, when a patient is declared brain-dead, their family is allowed a few hours or days to say their goodbyes before medical staff disconnect the body from a ventilator. This process hasn’t changed since I was a resident in the intensive-care unit nearly a decade ago. Due to patient-privacy rules, Emory hasn’t said what exactly happened in February following Smith’s apparently devastating and irreversible brain damage, but the standard procedure for a brain-dead patient clearly did not play out. Smith’s mother, April Newkirk, told reporters that the hospital instead kept Smith’s body on life support for more than four months without the family’s input or consent.
通常,当患者被宣布为脑死亡时,他们的家人被允许几个小时或几天说再见,在医务人员将身体与呼吸机断开连接之前。自从我十年前,我是密集型护理部门的居民以来,这个过程并没有改变。由于患者私人的规定,埃默里(Emory)并没有说史密斯(Smith)显然是毁灭性和不可逆转的脑部损害后2月发生的事情,但是对脑死亡患者的标准程序显然没有发挥作用。史密斯的母亲艾普尔·纽基克(April Newkirk)对记者说,医院未经家庭的投入或同意,医院将史密斯的尸体保留了四个多月。
In a statement last month, Emory said that its treatment decisions are based, in part, on “compliance with Georgia’s abortion laws.” Georgia’s LIFE Act, which has been in effect since the Supreme Court overturned Roe v. Wade, in 2022, grants full constitutional rights to any “unborn child with a detectable human heartbeat” (usually occurring around six weeks of gestation). This concept is known as fetal personhood, and in Smith’s case, it seems to have pushed doctors into an extraordinary—and extraordinarily troubling—situation.
埃默里(Emory)在上个月的一份声明中说,其治疗决策部分基于“遵守佐治亚州的堕胎法”。自从最高法院推翻Roev。Wade以来,佐治亚州的《生命法》(Georgia)的《生命法》(Life Act)在2022年推翻了Roev。Wade,授予任何“具有可检测到的人类心跳的未出生的儿童”(通常发生在妊娠六周左右)。这个概念被称为胎儿人格,就史密斯而言,它似乎使医生陷入了一个非同寻常的和非常令人不安的命运。
Four fundamental principles underlie health-care ethics: beneficence, non-maleficence, autonomy, and justice. In my experience practicing women’s reproductive health care, including abortion care, applying these principles simultaneously to the mother and the fetus can be—at the very least—fraught. The needs of the pregnant woman and the fetus are often in conflict, and many of the body’s physiological mechanisms to protect the fetus put even the healthiest pregnant woman at risk. Obstetricians often quip that their field is the hardest and most interesting because they must care for two patients at once, but any doctor who tries to truly uphold their ethical duties to two patients simultaneously risks landing in very murky territory.
卫生保健道德的四个基本原则:福利,非遗憾,自治和正义。根据我的经验,在练习妇女的生殖医疗保健,包括堕胎护理,同时将这些原则应用于母亲和胎儿,至少可以培养。孕妇和胎儿的需求经常处于冲突状态,保护胎儿的许多生理机制甚至使最健康的孕妇处于危险之中。产科医生经常打趣说他们的领域是最困难,最有趣的,因为他们必须一次照顾两名患者,但是任何试图真正地履行其道德职责的医生同时将其道德职责降落在两名患者身上,同时冒着降落在非常模糊的领土上的风险。
To be clear, Smith, as a brain-dead patient, was legally and medically deceased, so precepts about doing good and avoiding harm would not have applied to her, at least clinically speaking. But the ethical principle of autonomy applies even after a patient’s death. (Consider the United States’ strict consent laws around organ donation.) In the difficult cases when a patient—including a pregnant patient—is in such dire condition that she cannot speak for herself, a proxy decision maker, typically the next of kin, must be the one to make decisions about withdrawing care based on knowledge of the patient’s wishes or values. Some people might argue that a fetus, unable to speak for itself, should also be regarded as having some degree of autonomy; still, in Smith’s case, the fetus’s next of kin, not doctors, should have acted as a proxy decision maker.
需要明确的是,作为一名脑死亡的患者,史密斯在法律上和医学上都是死者,因此至少从临床上讲,对做好事和避免伤害的戒律不会对她施加。但是,即使在患者死亡之后,自治的道德原则也适用。(考虑到美国围绕器官捐赠的严格同意法。)在困难的情况下,当患者(包括怀孕的患者)处于这种糟糕的状态,以至于她不能为自己说话,她的代理决策者(通常是下一个亲戚)必须是根据对患者的愿望或价值观撤回护理的决定的人。有人可能会认为,胎儿也无法说话,也应该被视为具有一定程度的自治。尽管如此,就史密斯而言,胎儿的近亲,而不是医生,应该是代理决策者。
Yet Newkirk told reporters that prior to Chance’s birth, she was given no say in what happened to her daughter’s body, nor to the fetus inside her. Emory doctors simply followed what they believed the law prescribed. Since Smith’s case came to public attention last month, a spokesperson for the Georgia attorney general’s office has insisted that “there is nothing in the LIFE Act that requires medical professionals to keep a woman on life support after brain death.” But in all the months that Smith was kept on organ support (a more accurate term than life support), the attorney general refused to issue a formal legal opinion.
然而,纽基克(Newkirk)告诉记者,在Chance出生之前,她对女儿的身体发生了什么,也没有对她内心的胎儿发言。埃默里(Emory)医生只是遵循了他们认为的法律规定的内容。自从史密斯上个月引起公众关注以来,佐治亚州总检察长办公室的发言人坚持认为:“《生命法》中没有任何要求医疗专业人员在脑死亡后保持一名妇女的生活支持。”但是,在史密斯(Smith)保持器官支持(比生命支持更准确的几个月中),总检察长拒绝发表正式法律意见。
If Smith’s case sets a standard in Georgia and in other states with fetal-personhood laws, the implications could be far-reaching. Doctors might feel compelled to conduct a pregnancy test on any woman of reproductive age who dies in the hospital or is brought in dead. Some women might even sign an advance directive requesting that, should they die at any point in pregnancy, their organs be sustained so their fetus has a chance of survival. In the most extreme interpretation of the law, one can imagine an entire ward filled with dead women on ventilators, their bodies being used as incubators for tiny embryos.
如果史密斯的案件在佐治亚州和其他具有胎儿人格法律的州制定了标准,那么影响可能是深远的。医生可能会对任何在医院死亡或死亡的生殖年龄的妇女进行怀孕测试。一些妇女甚至可能签署提前指令,要求他们在怀孕的任何时候死亡,她们的器官可以维持,以便胎儿有生存的机会。在对法律的最极端解释中,人们可以想象一个整个病房里充满了死去的妇女,他们的身体被用作小胚胎的孵化器。
Read: The anti-abortion movement’s attack on wanted pregnancies
阅读:反堕胎运动对通缉怀孕的攻击
This image invokes a crucial debate about justice that already permeates the American health-care system. The United States spends extraordinary amounts of money on medical care at the extremes of life: neonatal intensive care on the one end, and ICU care for the elderly on the other. (As of Sunday night, Chance remains in the NICU. Newkirk has said that she hopes he will make it home, as most babies born at 27 weeks do, typically after weeks of intensive care.) In part, routine critical care for the very, very old and very, very prematurely born reflects a strong cultural pressure against assigning relative value to any individual life. But it does not always reflect the values of individual patients and their families. And it can raise uncomfortable questions about both benefits and costs—for example, how to measure the value of keeping one very sick patient alive versus, say, distributing large-scale public-health benefits to underserved populations.
该图像引起了关于正义的关键辩论,该辩论已经渗透到美国的医疗保健系统。在生活的极端,美国在医疗上花费了大量的钱:一端的新生儿重症监护,而ICU另一方面护理老年人。(截至周日晚上,纽基尔克(Newkirk)说,她希望他能回家,就像大多数在27周内出生的婴儿一样,通常是经过数周的重症监护。但这并不总是反映个人及其家人的价值。它可能会引起有关福利和成本的不舒服问题,例如,如何衡量使一个非常病的患者活着而不是为服务不足的人群分发大规模的公共卫生福利的价值。
Such questions become especially pointed if you consider how often the health-care system fails people before they reach the brink of death—and how it fails certain people more often, and more egregiously, than others. Research shows that doctors in the U.S. routinely ignore the health concerns of Black women such as Smith, and that Black mothers and their babies die at dramatically high rates compared with their white peers. Justice, then, is not only a question of how doctors assign value to a given human life, but also a question of whose voices they listen to, and whose voices are ignored or silenced. According to Newkirk, back in February, Smith went to Atlanta’s Northside Hospital complaining of severe headaches; doctors sent her home without imaging her brain. (Neither Northside nor Emory Healthcare responded to requests for comment.) A day later, her boyfriend found her struggling to breathe and called 911. She was rushed to a different hospital and at some point fell unconscious. She never woke up.
如果您考虑医疗保健系统在人们到达死亡的边缘之前的频率,并且如何使某些人更频繁,更令人生畏地失败,那么这些问题就会变得尤为明显。研究表明,美国的医生通常会忽略史密斯等黑人妇女的健康问题,而黑人母亲及其婴儿与白人同龄人相比以巨大的速度死亡。因此,正义不仅是医生如何将价值分配给给定的人类生活的问题,而且是他们倾听的声音以及其声音被忽视或沉默的问题。据纽基克(Newkirk)称,早在2月,史密斯(Smith)去了亚特兰大北区医院,抱怨严重头痛。医生将她送回家而没有成像她的大脑。(Northside和Emory Healthcare都没有回应置评请求。)一天后,她的男友发现她努力呼吸并打电话911。她被送往另一家医院,在某个时候昏迷了。她从不醒来。
As a doctor who cares for pregnant women, I know that patients rarely get to choose between a “right” and “wrong” decision. My job is to present all of the imperfect but ethically permissible options, and their implications for the fetus, to the person in front of me. Those options might include seeking treatment elsewhere if my care is limited by the law or other factors. But my years of practice have taught me that the patient, and the patient alone, must be the one to make that difficult, imperfect decision. This approach is a fairly good summary of how most abortion care works in the United States today. But it’s not how all doctors handle such choices. It certainly isn’t what happened at the time of Adriana Smith’s tragic death. Instead, Newkirk’s remarks indicate that no one explained to her exactly how doctors’ decisions may have been constrained by Georgia law, and no one suggested that she might transfer her daughter’s body to another hospital—even another state—where she might have had a say in those decisions.
作为照顾孕妇的医生,我知道患者很少在“正确”和“错误”的决定之间进行选择。我的工作是向我面前的人介绍所有不完美但道德上允许的选择及其对胎儿的影响。如果我的护理受到法律或其他因素的限制,这些选择可能包括在其他地方寻求治疗。但是我多年的实践告诉我,病人和患者仅是做出这一困难,不完美决定的人。这种方法是当今美国大多数堕胎护理如何工作的相当好的摘要。但这并不是所有医生处理此类选择的方式。当然,这不是阿德里亚娜·史密斯(Adriana Smith)悲惨去世时发生的事情。取而代之的是,纽基尔克(Newkirk)的言论表明,没有人向她确切解释医生的决定如何受到佐治亚州法律的约束,没有人建议她可以将女儿的尸体转移到另一家医院(甚至是另一个州),甚至是她在这些决定中可能有发言权。
Elizabeth Bruenig: Whose choice? Whose life?
伊丽莎白·布鲁尼格(Elizabeth Bruenig):谁的选择?谁的生活?
The case of Adriana Smith, though not about abortion, is very much about the ethics of choice. April Newkirk never publicly asked for her daughter’s body to be removed from organ support, but she did insist that the decision should have rested with her family. In an interview last week, Newkirk reiterated that what had happened to her daughter was a breach of autonomy. “I think all women should have a choice about their body,” she said. “And I think I want people to know that.”
阿德里亚娜·史密斯(Adriana Smith)的案例虽然与堕胎无关,但与选择的伦理非常重要。April Newkirk从未公开要求将女儿的尸体从器官的支撑中删除,但她确实坚持认为该决定应该依靠她的家人。在上周的一次采访中,纽基克重申,她女儿发生的事情违反了自治。她说:“我认为所有女人都应该选择自己的身体。”“而且我想我希望人们知道这一点。”